Menopause Treatment Clinic in Charleston, SC
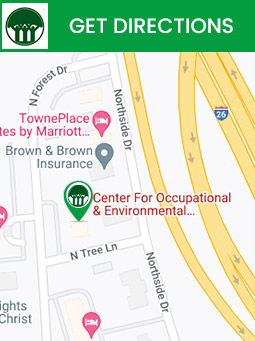
Menopause happens when the ovaries no longer release an egg every month and menstruation stops. Get comprehensive and specialized care at The Center for Occupational and Environmental Medicine (COEM). For more information, contact us today or book an appointment online. We are conveniently located at 7510 North Forest Drive North Charleston, SC 29420.


Table of Contents:
What is menopause?
Signs and symptoms of menopause: When does menopause start?
What causes menopause?
The three key stages of menopause
Bleeding after menopause: Is it normal?
What are hot flashes and how long will I keep having them?
What triggers a hot flash?
Can you take bioidentical hormones after menopause?
When should you visit your doctor for menopause treatment?
Our bodies go through many different changes throughout our lives and, for women, menopause is just one of them. Menopause is completely natural and normal, but it’s still important to keep yourself educated and prepared for this new life chapter
Menopause is the point in a woman’s life when her menstrual cycles come to an end. It’s often diagnosed after 12 months of not having a menstrual cycle and not being pregnant.
The main symptoms of menopause are:
• Irregular periods
• Hot flashes and night sweats
• Mood swings
• Forgetfulness
• Difficulty in sleeping
• Weight gain and slowed metabolism
• Change in libido
Menopause can occur in your 40s or 50s, although the average age in the United States is 51.
Menopause is a completely natural biological process. However, the physical and mental symptoms of menopause, such as hot flashes, can interrupt your sleep, reduce your energy, and impact your emotional health.
There are three main stages of menopause
1. Perimenopause or Pre-menopause
This phase typically starts about 4 to 8 years before the onset of menopause. When you reach pre-menopause, you will most likely start to experience some early menopausal symptoms, such as changes in your menstruation or mood swings.
2. Menopause
Menopause is a particular point in time that occurs when your periods stop and you do not have periods for twelve consecutive months.
3. Post-menopause
The term “post-menopause” means “after menopause.” You will continue to have menopausal symptoms during this period, and the symptoms typically persist two to seven years after menopause, although they might continue longer for certain people.
No. Any amount of vaginal bleeding after menopause is not normal, and you should get medical help if you are experiencing any bleeding after menopause.
Hot flashes are among the most common signs of menopause in women. It is a sudden feeling of heat. Hot flashes are not the same for everyone, and there is no apparent cause for them. The duration of hot flashes can also vary from person to person. For some people, hot flashes are a temporary symptom, while others can experience it for the rest of their life.
Some of the primary triggers of a hot flash are:
• Smoking
• Caffeine
• Alcohol
• Tight clothing
• Spicy foods
• Stress and anxiety
• Heat and hot weather
There’s no exact age limit for women to stop hormone replacement therapy which includes taking bioidentical hormones. Women aged above 60 can consider opting to continue hormone therapy to prevent persistent hot flashes, protect against osteoporosis, and avert any quality-of-life issues. However, before doing so, they would need an appropriate medical evaluation and counseling from a healthcare professional to understand the benefits and risks of the treatment.
It would be best to keep up with regular doctor visits during and after menopause as a preventive measure to avoid future complications.
If you are looking for the best board-certified gynecologist specializing in Functional Medicine near you, the Center for Occupational and Environmental Medicine can help you. Reach out to us or schedule an appointment with our expert OB/GYN doctors today. We serve patients from Charleston, Mt. Pleasant, Summerville, North Charleston SC, Ladson SC, Hanahan SC, James Island SC, John’s Island SC, Daniel Island SC, all of South Carolina, Nationally, and Internationally. Patients routinely fly into Charleston to be evaluated by COEM and to enjoy this beautiful city which is a Condé Nast and Travel and Leisure Top Domestic and International Tourist Destination.